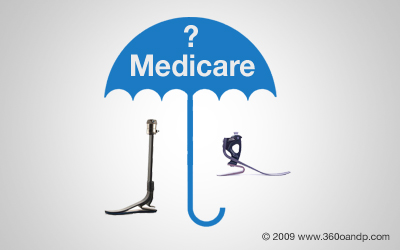
For the most part, Medicare provides excellent coverage for prosthetic services. Of course, that 20% coinsurance can really drain a beneficiary's saving's account. Many people assume, because they are on Medicare, the prosthetic coverage will be substandard. The opposite is actually true. Commercial insurance companies can impose a whole list of restrictive, and sometimes seemingly arbitrary, guidelines. Many commercial insurance companies will impose caps on care, allowing for as little as $1000.00 coverage for prosthetic items per year. Extremely large deductibles and exclusions for particular components or technologies, such as microprocessors, are also common.
Medicare bases its coverage guidelines on medical necessity. If the need is legitimate, there is sufficient records supporting medical necessity, the device will realistically benefit the user, and the physician is on board, providers are generally in the clear.
Coverage During Part A Stay
Medicare will pay prosthetic providers for most prosthetic equipment billed during the users Part A stay at a nursing facility. Some of the few exceptions of this rule are:
· Partial foot prosthetic codes: L5000-L5020
· Codes for post surgical application of rigid dressings: L5400-L5460
· Partial hand prosthetic codes: L6000-L6020
· A Vertical loading pylon foot: L5987
· Replacement on minor components: L7510
· Labor: L7520
· Most soft goods, including socks and shrinkers: L7520-L8499
For the codes listed above, prosthetic providers cannot directly bill Medicare during a users Part A stay. This is included in Medicare's payment to the facility and the facility would be responsible for payment to the provider.
Frequency of Replacement
For prosthetic items, Medicare is more concerned with medical necessity than time frames. Medicare will cover an item, regardless of time frame, if the physician orders the prosthesis or prosthetic component due to:
· The user has experienced a change in condition
· The device has suffered irreparable wear or damage
· The cost for repairs exceeds 60% of the cost of replacement
Other Requirements
Prosthetic items must be:
· Eligible for a defined Medicare benefit category
· Be reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member, and
· Meet all other applicable Medicare statutory and regulatory requirements
The user of the proposed device or components must:
· Be able to reach or maintained a defined functional states within a reasonable period of time, and
· Be motivated to ambulate
Certain prosthetic components will only be covered for users with certain functional levels. Functional levels range from 1-4. An individual with no desire or potential to ambulate, or transfer only, would be a level 0. For a level 0, prosthetic components would not be covered. For an item like a FlexFoot, L5980, the user must be a functional level 3, or active community walker that walks at a variable speed over uneven terrain.
Additional Limitations
There are a handful of components that are subject to more strict guidelines. For example:
· No more than 2 socket inserts (such as L5679 or L5673) can be allowed at the same time for a single prosthesis.
· No more than two diagnostic (test) sockets (such as L5624 or L5620) will be considered medically necessary for fabrication of a single prosthesis, unless there is significant medical justification in the records to justify the need.
· Some components, such as L5980 or L5631 cannot be used on an initial prosthesis.
Unfortunately Medicare does not provide orthotic and prosthetic providers with pre-authorization or a pre-determination of coverage. That is why it is imperative that providers remain extremely familiar with Medicare guidelines. These guidelines can be found in the DMERC Supplier Manual.
Source: 2006 Region C DMERC Supplier Manual